Safety measures to prevent contamination when using a Platelet Rich Plasma (PRP) kit are crucial to ensure the sterility and safety of the PRP product. Contamination can lead to infections or other adverse effects for the patient. Here are the key safety measures:
- Aseptic Technique: Healthcare providers should strictly adhere to aseptic technique during PRP preparation and administration. This involves thoroughly disinfecting hands, surfaces, and equipment, as well as wearing sterile gloves and using sterile drapes and barriers.
- Clean Environment: Perform PRP procedures in a clean, controlled environment, such as an operating room or a sterile procedure room. Minimize the risk of airborne and surface contaminants.
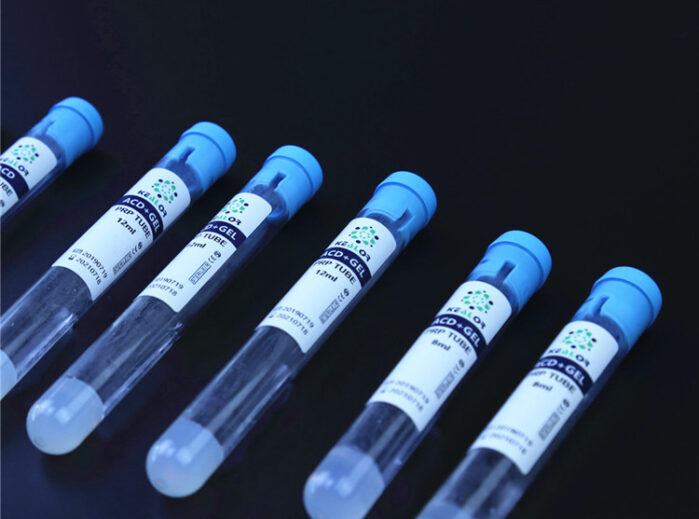
- Sterile Equipment: Ensure that all equipment, including needles, syringes, centrifuge tubes, and collection containers, is sterile and single-use if specified by the manufacturer. Use disposable items when possible to prevent cross-contamination.
- Sterile Packaging: PRP kits often come in sterile packaging. Maintain the sterility of the kit until it is ready to be used, and open the packaging only in the sterile field.
- Hand Hygiene: Healthcare providers should practice thorough hand hygiene by washing hands with soap and water or using an alcohol-based hand sanitizer before and after the procedure.
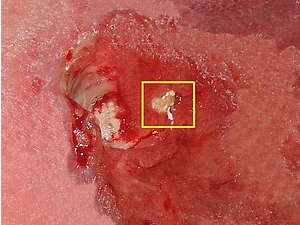
- Patient Skin Preparation: Properly clean and disinfect the patient’s skin at the site where the blood will be drawn or the PRP will be injected to minimize the risk of introducing pathogens.
- Waste Management: Dispose of used needles, syringes, and other disposable items in designated sharps containers. Properly dispose of waste following biohazard and medical waste disposal regulations.
- Use of Personal Protective Equipment (PPE): Healthcare providers should wear appropriate PPE, including gloves, gowns, masks, and eye protection, to protect themselves and the patient from potential contamination.
- Preventing Cross-Contamination: Avoid cross-contamination between PRP components (e.g., platelets, plasma) by using separate, sterile containers, syringes, and other equipment for each step of the procedure.
- Proper Cleaning and Maintenance of Equipment: Maintain and clean centrifuges, processing equipment, and any reusable items following manufacturer guidelines and recommendations.
- Monitoring and Quality Control: Regularly monitor and verify the sterility and quality of PRP kits and components. Perform quality control checks, such as verifying expiration dates and inspecting for damaged packaging.
- Training and Education: Ensure that healthcare providers performing PRP procedures are trained and educated in aseptic techniques and the specific procedures associated with the PRP kit being used.
- Documentation: Maintain thorough documentation of the PRP procedure, including the lot numbers of PRP kit components, patient information, and any deviations or complications encountered during the procedure.
- Adherence to Regulatory Standards: Follow regulatory standards and guidelines related to PRP preparation and administration in your region or country.
By rigorously adhering to these safety measures, healthcare providers can minimize the risk of contamination during PRP procedures, ensuring the safety and well-being of patients and optimizing the therapeutic benefits of PRP therapy.