Platelet-rich plasma (PRP) is plasma containing high concentrations of platelets obtained by centrifugation of whole blood. These growth factors have the ability to promote cell proliferation. These growth factors have various effects on cell proliferation, differentiation, chemotaxis and stimulation of vascularisation.
Preparation of PRP
PRP preparation: PRP is extracted from whole blood by density gradient centrifugation. The principle is that there are many ways to make PRP depending on the sedimentation coefficient of the individual components of the blood, and the concentration and activity of platelets in PRP varies with the number of centrifugations, centrifugal force and centrifugal time.
The main components of PRP
Platelet-derived growth factor: Platelet-derived growth factor, first found in platelets, is a cationic polypeptide that is heat- and acid-resistant and readily hydrolysed by trypsin, and was one of the first growth factors to appear in fracture sites. It is efficiently expressed in traumatic bone tissue, causing osteoblast chemotaxis and proliferation, and increases collagen synthesis and promotes osteoclast resorption, thereby promoting bone formation.
Transforming Growth Factor β: Transforming Growth Factor β is a 2-chain peptide that acts in a paracrine or autocrine manner on fibroblasts, bone marrow stromal stem cells and preosteoblasts, stimulating the proliferation of osteoblasts and preosteoblasts and collagen fibre synthesis, acting as a chemotactic factor to resorb bone progenitor cells into the injured bone tissue and inhibiting the formation and resorption of osteoclasts.
Insulin-like growth factor: Insulin-like growth factor is a single-chain polypeptide that binds to receptors in bone and activates tyrosine proteases after receptor autophosphorylation, leading to phosphorylation of insulin receptor substrates, thereby regulating cell growth, proliferation and metabolism, which stimulates osteoblasts and pro-osteoblasts and promotes cartilage and bone matrix formation. On the other hand, it plays an important role in bone remodelling coupling by mediating the differentiation and formation of osteoblasts and osteoclasts and their functional activity.
Epidermal growth factor: EGF is a potent cytokine-promoting factor that stimulates the division and proliferation of many types of tissue cells in the body, while promoting matrix synthesis and deposition, fibrous tissue formation, and continued transformation into bone to replace bone tissue formation. Another factor involved in fracture repair is the activation of phospholipase A, which promotes the release of arachidonic acid from epithelial cells and promotes prostaglandin synthesis by regulating the activity of cyclooxygenase and lipoxygenase, which have a dual role in early bone resorption and later bone formation. This suggests that epidermal growth factor is involved in the fracture healing process and can accelerate fracture healing.
Vascular endothelial growth factor: VEGF is a dimeric glycoprotein that binds to the surface receptors of vascular endothelial cells through autocrine or paracrine secretion to promote endothelial cell proliferation and induce neovascularisation. The establishment of neovascularisation, the supply of oxygen to the fracture end, the provision of nutrients, the transport of metabolic waste and the provision of a favourable microenvironment for local bone regeneration and metabolism. Secondly, under the action of VEGF, osteoblasts differentiate, alkaline phosphatase activity is enhanced, and local calcium salts are deposited, promoting fracture healing. In addition, VEGF indirectly promotes fracture healing by improving the blood supply to the soft tissues surrounding the fracture and promoting cartilage tissue repair.
Current use of PRP
Regeneration of bone defects: Whitman et al. were the first to investigate the use of PRP to repair defects, and the current view is that the combined effect of the high concentrations of growth factors in PRP stimulates osteogenesis and accelerates bone repair. However, because PRP has not been studied in depth at the cellular-molecular level, there have been conflicting reports on the effects of PRP. Aghaloo et al. used autologous bone plus PRP to repair rabbit cranial defects and concluded by comparison that the addition of PRP did not significantly promote bone growth. Furthermore, some scholars believe that the overexpression of growth factors may be associated with mesenchymal tumours and dysplasia. The reasons for this may be analysed as follows: 1. The effect of PRP on bone regeneration is significantly time-dependent and dose-dependent. 2. The transforming growth factor beta in PRP is homologous to bone morphogenetic proteins and they compete for receptors, thus inhibiting the activity of bone morphogenetic proteins, which in turn reduces the differentiation of bone marrow mesenchymal cells with osteogenic potential to bone and chondrocytes. 3. In an excessive concentration of platelets in the environment, excessive inhibition and cytotoxicity can affect growth factor activity.
In spinal fusion: Lowery et al. demonstrated the ability of PRP to promote early osseointegration. In a clinical study applied to anterior lumbar fusion, PRP was found not to promote vertebral fusion, which he attributed to the following possible causes: 1. the technique used to prepare the PRP gel reduced platelet activity.
- the aggregation of platelets during manufacture affected platelet activity.
- the absence of a good platelet
- no determination of the duration of platelet growth factor preservation and optimal application time.
- the growth factor may over-stimulate the inflammatory response, leading to fibrous tissue deposition rather than bone formation.
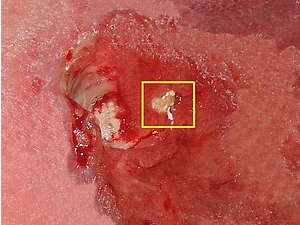
With regard to difficult-to-heal wounds: platelet-derived growth factors can increase infiltration of traumatic fibroblasts and inflammatory cells, increase collagen synthesis in wound tissue and promote granulation tissue growth. Guo Yanjie et al. obtained good follow-up in the treatment of chronic osteomyelitis wounds with PRP and concluded that PRP could promote the repair of difficult-to-heal wounds. Transforming growth factor beta is involved in many inflammatory responses and tissue repair in the body and is a multifunctional basic anti-inflammatory cytokine in the body. Insulin-like growth factor 1 can act synergistically with platelet-derived growth factors to increase epidermal and endothelial regeneration. Vascular endothelial growth factor A has a role in promoting vascular renewal and enhancing vascular permeability. VEGF C is a chemotactic and divisive factor for endothelial cells and may also have a role in promoting lymphatic neoplasia in the blood vessels. VEGF D is similar to VEGF C in that it promotes vascular and lymphatic vessel neogenesis.
The relationship between growth factors and wound healing, the complex regulatory relationships between growth factors, the mechanisms of growth factor regulation of cell differentiation, and the optimal environment for wound healing, including blood flow, oxygen partial pressure, humidity and pH, and the release of growth factors need to be further investigated.
In terms of tissue engineering, Lucarelli et al. used allogeneic bone compounded with PRP, collagen and bone marrow stromal stem cells to construct tissue-engineered bone to repair a defect in the middle part of the sheep’s toe, and the experimental group showed significant new bone formation and better bone remodelling and neovascularisation than the control group after 4 months. liquid, combined with thrombin to form a gel) and obtained better results in ectopic osteogenesis experiments, with the resulting new bone forming not only with good maturation but also with significant neovascularisation.
Other disciplines: platelets have various coagulation factors adsorbed on their surface, such as plasma fibrinogen and prothrombin, etc. In addition, platelets contain: “endogenous coagulation factors” which are released through certain circumstances, resulting in an increase in the concentration of the corresponding coagulation factors in plasma and a shortening of the prothrombin time and thromboplastin time assay. The use of PRP for colonic anastomosis, especially in patients with poor wound healing, was found to have improved anastomosis results.
Advantages of PRP applications
PRP has clear advantages in various clinical disciplines
- PRP is free of disease transmission and immune rejection, which fundamentally eliminates the risk of disease transmission between patients.
- PRP contains a high concentration of various growth factors, the ratio of each growth factor is similar to the normal ratio in the body and has an optimal synergistic effect. This compensates to some extent for the poor stimulation of osteogenesis by a single growth factor and meets the need for the growth factors required for early bone healing.
- PRP gel is adhesive, which facilitates graft adhesion, prevents the loss of growth factors and maintains a high local concentration of growth factors.
- PRP has a pro-coagulant effect, stimulating soft tissue regeneration and promoting early wound healing.
- The growth factors contained in PRP do not enter the cells or the nucleus, which accelerates the normal healing process.
- PRP is simple to produce and causes little damage to the patient, as it can be produced by simply taking blood from the patient’s vein.
Conclusion and outlook
There are still a number of issues that need to be addressed with regard to the clinical use of PRP
- There is no unified standard for PRP production, and there is a need to establish an efficient and stable PRP production method, a special kit approved and tested by the relevant national authorities, and a sterility requirement to provide quality assurance for the wide application of PRP.
- Different methods of making PRP cause much platelet destruction and insufficient extraction purity, making the concentration of various growth factors in PRP vary greatly, as well as the activity of various factors, biological effects, such as the mechanism of promoting bone repair, have not been fully elucidated.
- The relationship between the amount of various growth factors in PRP and the optimal dose to promote bone regeneration, as well as the mechanisms of growth interactions, have not been fully elucidated.
- Some scholars are sceptical about the effectiveness of PRP in promoting bone repair.
PRP is currently being studied in small-scale oral and maxillofacial and cranial defects, but there is a lack of experimental data on the application of PRP in orthopaedics, especially in bone defects of the extremities and in large segments of bone defects and bone discontinuities.