Why do wounds have the ability to heal themselves?
The skin is the largest organ of the body and one of the body’s first lines of immune defence. It is broadly divided into an epidermis, a dermis and a subcutaneous tissue layer, which contains a wealth of glands, blood vessels and nerves, among other issues. When the skin is exposed to external injury-causing factors, the skin structure is destroyed and a certain amount of soft tissue is lost, resulting in loss of normal skin integrity and impaired function, resulting in a wound.
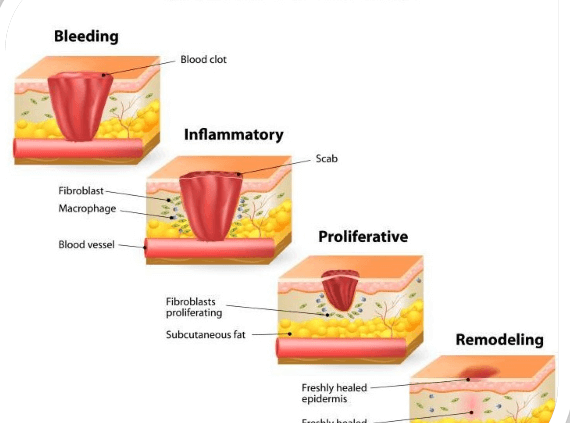
Normal skin has a certain degree of repair and regeneration, usually through the haemostasis phase, the inflammatory response phase, the migration and accretion phase and the maturation phase, each of which does not occur completely independently of the other, but actually overlaps with the other.
In other words, after the formation of a skin defect, the repair of the wound mainly consists of the processes of granulation, re-epithelialisation and scar formation, as well as healing and reconstruction of the wound. Modern medicine recognises that skin defect repair is a dynamic process involving complex interactions between multiple cells, growth factors and the extracellular matrix.
Why are some wounds difficult to heal?
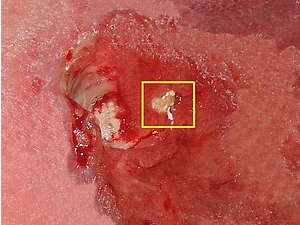
However, when the skin repair and regeneration process is blocked, normal skin repair and regeneration cannot be completed, resulting in delayed healing, non-healing or recurrent soft tissue skin defects and chronic wounds. Common chronic wounds include pressure sores, venous calf ulcers, arterial ulcers, neurotrophic ulcers and diabetic foot ulcers. Chronic wounds often involve multiple tissues at the same time, including epidermal, vascular muscle and nerve tissues.
Pressure ulcers (PU), also known as pressure ulcers, are common chronic clinical wounds. The European Pressure Ulcer Advisory Committee. (EPUAP) defines a pressure ulcer as a localised injury to the skin and/or subcutaneous tissue, usually located at the bony process, caused by pressure or pressure combined with shear forces.
Current treatment options for chronic wounds have the most important goal of addressing the causative factors, with the remaining treatment modalities including removal of necrotic tissue, relieving pressure on the wound, maintaining a wet environment on the wound, treating and preventing wound infection and enhancing nutritional status. Despite this, many chronic wounds still have difficulty healing and place heavy stress and burden on patients and their families.
Platelet-rich plasma for chronic wounds
As basic research and clinical applications of autologous platelet-rich plasma (PRP) continue to expand, the clinical efficacy of PRP in the treatment of chronic wounds is emerging. PDGF, Epidermal Growth Factor (EGF), Transforming Growth Factor-β (TGF-β), Vascular Endothelial Growth Factor (VEGF), etc., which facilitate the repair and regeneration of damaged tissues and tissue vascularisation, removal of necrotic tissues, modulation of inflammatory levels, relief of wound pain, and promotion of nerve axon regeneration and increased tissue neurotrophy.