What exactly is PRP?
PRP: The full name of PRP is Platelet-rich plasma, which is a plasma containing a high concentration of platelets prepared from your own blood. It has many names, such as PRC (Platelet-rich concentrate), or APG (Autogenous platelet gel), and PRGF (Plasma rich in growth factor).
A brief history of PRP
The use of PRP technology goes back a long, long way.
- The first discoveries of multiple growth factors in human blood were made in 1984
- In 1993, the concept of PRP was introduced and it was found to be rich in platelets
- In 1997, the Swiss state discovered that it had haemostatic properties
- In 2000, PRP was gradually introduced in surgery, burns and dermatology
Composition of PRP components
The most important component of PRP is, of course, P, or platelets. Platelets are cytoplasmic fragments of megakaryocytes, which belong to the category of white blood cells and are formed in the bone marrow. Platelets are rich in cell growth factors such as platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-beta), vascular endothelial growth factor (VEGF) and insulin-like growth factor (IGF), among others, as well as fibrin and small amounts of leucocytes.
The PRP technique is based on obtaining PRP and adding a coagulant (marketed as an activator and commonly used as a 10% calcium chloride solution and thrombin) to form a gel that is used to repair and promote tissue regeneration for clinical treatment purposes.
PRP has four main properties
1) Release of bioactive factors
With a pH value of 6.5-6.7, the addition of appropriate activators will promote wound and tissue healing and cell regeneration cytokines
2) The active factors secreted have a natural ratio
The concentration ratio of various growth factors is close to the normal ratio in the body, and each growth factor interacts with each other
3) Easy to activate and inactivate
After activation, they exert biological effects. It can be prepared as platelet gel, but platelets are easily damaged, resulting in the ineffectiveness of a large number of growth factors
4) PRP has a concentration effect
Platelet concentration is 3-17 times higher than that of whole blood. After exceeding the upper limit of cytokine concentration, the proliferative effect is reduced
How is PRP prepared?
The former is highly automated, but the equipment is expensive, so centrifugation is currently the main method of preparation. There are also commercially available specialised sleeves for rapid preparation of PRP, which greatly improve the enrichment factor and harvest rate.
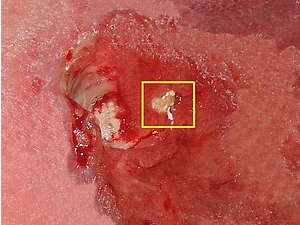
Without going into the specific steps of PRP preparation, the various components of the blood can be separated after centrifugation. Platelets are light in specific gravity and are mostly retained in the upper plasma layer, which can be separated out to give platelet-rich plasma, yielding over 70% of platelets in whole blood.
When PRP meets stem cells?
The body’s self-healing needs to be regulated by a variety of growth factors, and PRP contains a variety of growth factors. Therefore, if PRP is used in combination with stem cells, it can create and improve the microenvironment for stem cell growth, further increasing the survival rate of stem cells and improving the therapeutic efficacy.
Currently, the combination of PRP and stem cells is commonly used in the following areas:
- Combination of PRP and adipose stem cells for knee osteoarthritis
PRP composite scaffold material has high osteogenic induction activity and can promote bone tissue healing. On its own, it also has anti-inflammatory and cartilage regenerative effects and can repair small cartilage defects. If the PRP composite scaffold is combined with stem cells for knee osteoarthritis treatment for cartilage defects, it can provide a better microenvironment for stem cell growth (promoting blood supply and reducing local inflammatory response) and can promote the synthesis of cartilage matrix, improving the therapeutic effect of stem cells in knee osteoarthritis.
- Combination of PRP, adipose tissue and adipose stem cells in medical aesthetic applications
It is mainly used for facial fillers, breast fillers and facial rejuvenation. The key to the survival of autologous fat grafts is the establishment of a vascular network around the graft, and theoretically, anything that promotes vascular regeneration can improve the survival of transplanted fat grafts; PRP combined with adipose stem cells can promote vascular growth, which means that the blood supply around the fat tissue can be increased in fat fillers, improving the survival rate of the fat tissue transplanted.
Conclusion
It is generally accepted that the primary role of PRP is to accelerate healing in the early stages, reduce pain and swelling and reduce complications. This is attributed to the anti-inflammatory effect of PRP. Although the end result is similar, this accelerated and enhanced healing time reduces complications of the procedure, such as pain, infection, etc.