The Comparison between the Composition of 100% Autologous Serum and 100% Platelet-Rich Plasma Eye Drops and Their Impact on the Treatment Effectiveness of Dry Eye Disease in Primary Sjogren Syndrome
Dry eye disease (DED) is a common ocular surface disorder, characterized by symptoms such as dryness, burning, itching, and foreign body sensation. One of the main causes of DED is primary Sjogren syndrome (pSS), an autoimmune disorder that affects the salivary and lacrimal glands, leading to decreased tear production and quality. Various treatments for DED have been developed, including the use of autologous serum (AS) and platelet-rich plasma (PRP) eye drops.
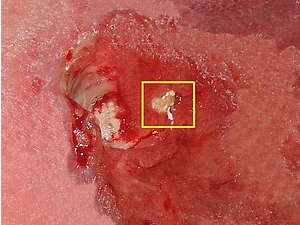
AS and PRP are both derived from the patient’s blood, but they differ in their preparation methods and composition. AS is obtained by separating the serum fraction of blood, which contains various growth factors, cytokines, and other components that promote tissue repair and regeneration. PRP, on the other hand, is obtained by centrifuging whole blood, which separates the platelet-rich fraction, containing high concentrations of growth factors and cytokines.
Several studies have investigated the effectiveness of AS and PRP eye drops in the treatment of DED in pSS patients. One study compared the composition of 100% AS and 100% PRP eye drops and found that PRP contained significantly higher concentrations of platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF) than AS. These growth factors play a crucial role in tissue repair and regeneration, making PRP eye drops potentially more effective than AS eye drops in promoting the healing of the ocular surface in DED patients.
Another study compared the effectiveness of AS and PRP eye drops in the treatment of DED in pSS patients and found that both treatments were effective in improving tear film stability and reducing ocular surface inflammation. However, the study also found that PRP eye drops were significantly more effective than AS eye drops in improving ocular surface disease index (OSDI) scores, Schirmer test scores, and tear break-up time (TBUT). These findings suggest that PRP eye drops may be a more effective treatment for DED in pSS patients than AS eye drops.
In conclusion, the use of PRP eye drops may be a more effective treatment for DED in pSS patients than AS eye drops due to the higher concentration of growth factors and cytokines present in PRP. Further studies are needed to investigate the long-term effectiveness and safety of PRP eye drops and to optimize the preparation methods and dosages of PRP eye drops for the treatment of DED in pSS patients.