Platelet-Rich Plasma (PRP) therapy has become a widely discussed topic in the medical field, especially in orthopedics and sports medicine. One aspect that sparks debates is whether platelets need to be activated before injecting them into the knee joint. Understanding the role of platelet activation in PRP knee injections is crucial in determining its necessity and its impact on treatment outcomes. In this article, we’ll explore the reasons behind platelet activation, its potential benefits, and whether it’s a must for successful knee injections.
Platelet-Rich Plasma Therapy: An Overview
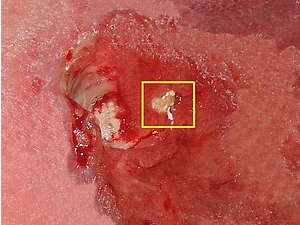
PRP therapy involves drawing a small amount of the patient’s blood, spinning it in a centrifuge to concentrate platelets and growth factors, and then injecting this solution into the affected area, such as the knee joint. Platelets are rich in growth factors that are believed to stimulate tissue repair and regeneration.
The Role of Platelet Activation
Platelet activation refers to the process of inducing the release of growth factors from the platelets. This step is sometimes performed before injecting PRP into the treatment site. Platelet activation can be achieved through various methods, such as using calcium chloride, thrombin, or exposure to collagen.
Benefits of Platelet Activation:
- Enhanced Growth Factor Release: Activated platelets release a higher concentration of growth factors, potentially accelerating the healing process.
- Immediate Effect: Some proponents of platelet activation argue that it might lead to more immediate therapeutic benefits.
- Enhanced Clot Formation: Activated platelets can aid in clot formation, which might be beneficial in cases of bleeding or to aid wound healing.
Is Platelet Activation Necessary for Knee Injections?
The necessity of platelet activation for knee injections is a topic of ongoing discussion and research. While some practitioners argue that activating platelets amplifies the therapeutic effects of PRP, others believe that the activation process might degrade certain growth factors or lead to the production of pro-inflammatory agents.
Several studies have shown positive results with both activated and non-activated PRP in knee injections, indicating that both methods can be effective. The choice between activated and non-activated PRP might depend on the specific goals of the treatment, the patient’s condition, and the medical professional’s expertise.
Considerations and Factors to Keep in Mind:
- Treatment Goals: Consider whether immediate effects are a priority or if gradual tissue regeneration is preferred.
- Patient’s Condition: The severity of the knee issue and the patient’s overall health play a role in deciding the optimal treatment approach.
- Practitioner’s Experience: The medical professional’s familiarity with both activated and non-activated PRP can guide the treatment decision.
The question of whether platelet activation is necessary for knee injections is not easily answered with a definitive “yes” or “no.” Both activated and non-activated PRP injections have shown positive outcomes in various cases. Deciding whether to activate platelets depends on multiple factors, including treatment goals, patient condition, and the practitioner’s expertise.
Ultimately, the decision should be made in consultation with a qualified medical professional who can evaluate your specific situation and tailor the treatment plan to your needs. Whether activated or non-activated, PRP therapy offers a promising avenue for knee joint rejuvenation and recovery, potentially providing relief for those seeking non-surgical options for knee issues.